How can I possibility make that statement? Two recent best-selling diet books have maintained that gluten makes us fat and dumb (1,2). Billions of dollars are spent on gluten-free (but carbohydrate-rich) food products. And people feel better when they don’t eat bread.
Before explaining my statement, let me make two things very clear. First, I am not a big believer in bread. In 1997, in a Time magazine interview I said, “If all the bread left the face of the earth, we would have a much healthier planet.” (3) I stand by that statement.
Second, gluten “sensitivity” is not celiac disease. Celiac disease is a clinically proven autoimmune response to the proteins in gluten (4). I know since my wife has severe celiac disease.
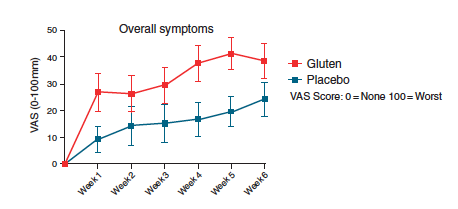
However gluten sensitivity is different. Most of the people who pretend to be experts in gluten sensitivity usually have no background in gastrointestinal research. After all, why try to back up your claims with real research that is very difficult to do? So it came as a great initial salvation to those people when a real expert from Australia published a paper indicating that gluten sensitivity may exist but with no clues to the mechanism (5). In this study subjects with irritable bowel syndrome (IBS) and no evidence of celiac disease were put on a gluten-free diet for six weeks and then either challenged daily with muffins and bread either containing gluten (16 grams per day) or without gluten. Even though both groups were on a gluten-free diet, they were both having more symptoms, although the group getting the extra gluten had more symptoms of IBS, including being more fatigued than the control group (5).
What was also strange about the results of this study was there were no differences in the intestinal inflammation or any increase in the permeability of the intestinal wall in either group. This caused the researchers to ponder if they had been too simplistic in their experimental design. So they went back to do another experiment in which a diet that was far more rigorous in reducing other potential food allergens, such as FODMAPs, which stand for Fermentable, Oligo-, Di-, Monosaccharides And Polyols. These are poorly absorbed short-chain carbohydrates, which means that many of these dietary carbohydrates reach the colon where the trillions of bacteria are waiting to begin fermenting them. FODMAPs are found in foods, such as those containing free fructose (found in apples, cherries, pears, asparagus, artichokes, etc.), foods that can be easily broken down into free fructose (such as high-fructose corn syrup and table sugar), free lactose (found in milk, yogurt, soft cheeses, etc.), polymers of fructose known as fructans (found in peaches, artichokes Brussels sprouts, fennel, onion, wheat, barley, and rye), polymers of galactose known as galactans (found in legumes, chickpeas, lentils, etc.) and polyols (found in apricot, avocado, blackberries, plums, cauliflower, mushrooms, snow peas, etc.). This is a lot more complex dietary undertaking than putting all of your bets on gluten (6).
So when the researchers repeated their experiment and removed many of the FODMAPs from the diet of the sufferers with “gluten sensitivity” and then added back bread and muffins consisting of either high gluten (16 grams per day), low gluten (2 grams per day), or a placebo, they got a very different response as shown below (7).
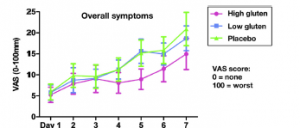
Now you get a very different picture than the earlier study in which the researchers had not removed many of the FODMAPs from the diets of their subjects. Furthermore, there was no increase in fatigue in those getting the gluten compared to the placebo, even though more than half of the subjects had the genetic susceptibility marker for celiac disease (DQ2 or DQ8 positive HLA), and a quarter of them had anti-bodies to gliadin (one of the proteins in the overall family of protein collectively called gluten).
These new results with the low-FODMAPs diet led the researchers to conclude: In a placebo-controlled, cross-over rechallenge study, we found no evidence of specific or dose-dependent effects of gluten in patients with non-celiac gluten sensitivity placed on diets low in FODMAPs. That’s a mouthful, but in essence the benefits of a gluten-free diet may not be the removal of gluten but the removal of various FODMAPs found in the wheat, rye, and barley that just happen to also contain gluten.
What remains unknown is whether it is the FODMAPs or a unique bacteria composition in the guts of the “gluten-sensitive” people interacting with the FODMAPs that can cause the problems that lead to IBS and the designation of being “gluten-sensitive”.
However one thing is certain: This new research will not stop the continuing flow of “gluten-free” products rich in carbohydrates coming from the food industry and more popular diet books “discovering” the real reason we are getting fatter and dumber. Maybe I was on the right track in 1997 when I stated that bread removal is not such a bad idea for mankind. That’s because I also believe that it is increased diet-induced inflammation, not simply gluten, that is the real cause of our growing epidemics of obesity, type 2 diabetes, and Alzhemier’s.
References:
- Davis W. Wheat Belly: Lose the Wheat, Lose the Weight, and Find Your Path Back to Health. Rodale Books. Erasmus, PA (2011).
- Perlmutter D. Grain Brain: The Surprising Truth about Wheat, Carbs, and Sugar-Your Brain's Silent Killers. Little, Brown and Company. New York, NY (2013).
- Ratnesar R. “Against the grain.” Time. December 15, 1997 (1997).
- Fasano A. Gluten Freedom: The Nation's Leading Expert Offers the Essential Guide to a Healthy, Gluten-Free Lifestyle. Wiley. New York, NY (2014).
- Biesiekierski JR, Newnham ED, Irving PM, Barrett JS, Haines M, Doecke JD, Shepherd SJ, Muir JG, and Gibson PR. “Gluten causes gastrointestinal symptoms in subjects without celiac disease: a double-blind randomized placebo-controlled trial.” Am J Gastroenterol 106:508-514 (2011).
- Gibson PR and Shepherd SJ. “Food choice as a key management strategy for functional gastrointestinal symptoms.” Am J Gastroenterol 107:657-666 (2012).
- Biesiekierski JR, Peters SL, Newnham ED, Rosella O, Muir JG, and Gibson PR. “No effects of gluten in patients with self-reported non-celiac gluten sensitivity after dietary reduction of fermentable, poorly absorbed, short-chain carbohydrates.” Gastroenterology 145:320-328 (2013).






Let Us Know What You Thought about this Post.
Put your Comment Below.